Photo by www.dailymail.co.uk
 A major breakthrough by British scientists could bring new hope for women facing the heartbreak of infertility.
A major breakthrough by British scientists could bring new hope for women facing the heartbreak of infertility.
For the first time a team has managed to grow hundreds of eggs in the laboratory using a new technique which could help cancer patients whose treatment can leave them infertile.
It would also allow thousands more women to wait until middle age to have children.
The scientists from Edinburgh University have shown that immature eggs can be frozen, grown and matured in the lab.
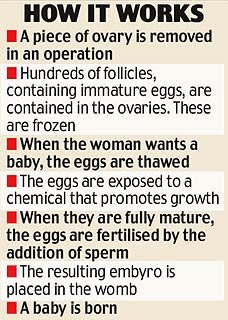
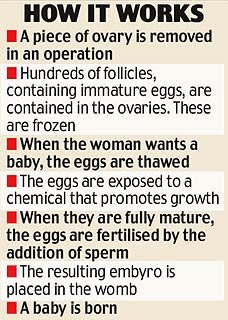
The process could lead to women having pieces of ovary containing the immature eggs removed and stored. Much later on, they could be thawed, fertilised and finally implanted into the womb.
The breakthrough, which comes as MPs prepare to debate the controversial Human Fertilisation and Embryology Bill, raises again the ethical debate surrounding the freezing of eggs.
Some say it is morally wrong for a woman to do so and have them fertilised years later in order to delay having children while she pursues a career.
However, scientists hope the new process will revolutionise fertility preservation for women because it will allow them to store many more eggs than they can under traditional IVF techniques.
And, because immature eggs survive the freezing process much better than the mature ones used in IVF, it is much more likely that older women will be able to conceive using them.
It brings forward the prospect that thousands of women will use the technique to side-step the menopause, delaying motherhood for the sake of their careers.
The process, which could be available in five years, also provides hope for cancer sufferers who at the moment are often left infertile following chemotherapy and radiotherapy.
Powerful anti-cancer drugs can destroy follicles in the ovaries, wiping out any possibility of women having children.
At the moment, these women have a piece of ovary removed, frozen and then re-transplanted after their cancer treatment. But there is always the danger that the cancer could be reintroduced by the implant.
The new technique means women's immature eggs contained in the patch of ovary could be grown in the lab and then screened for cancer before being used in IVF treatment.
There are also hopes it will provide a rich source of eggs for scientists to study for clues on ways to treat a range of diseases.
There is a shortage of human eggs for medical research, and if the technique works it would bypass the controversy over the use of animal-human 'hybrid' embryos.
The Human Fertilisation and Embryology Bill, which MPs are due to debate next month, would allow scientists to use these embryos in medical research, but many MPs plan to vote against.
The research, carried out by an Edinburgh University team led by Dr Evelyn Telfer, is published today in the journal Human Reproduction.
"This is a significant step in developing immature eggs to maturity outside the body," said Dr Telfer.
"Women who face infertility as a result of chemotherapy, or who want to put their biological clock on hold, could benefit from this system.
"However, there is a lot more research to be carried out before this technique could be safely applied within a clinical setting."
Last year, Canadian scientists announced the first birth of a child created from a human egg matured in the laboratory.
However, they did not use the same "primordial follicles" studied by the researchers from Edinburgh.
These are the tiny egg-bearing pockets within the ovaries that are present in their millions at birth, but gradually die off over the course of a woman's life.
They represent a woman's fertility "battery" which once depleted cannot be recharged.
Many remain dormant, but some go on to mature and eventually release their eggs in preparation for fertilisation.
For the first time, the team led by Dr Telfer has succeeded in growing primordial follicles to a late stage of maturation in the lab.
They took pieces of ovary containing the follicles from six volunteer women who were giving birth by caesarean section.
These were then exposed to a chemical that promotes growth, similar to the one that functions in the ovaries.
Around a third of them survived and went on to reach the advanced 'antral' stage of development.
At this stage, the follicles are filled with fluid and contain eggs almost ready to be fertilised.
It means that it could soon be possible to grow hundreds of eggs in the laboratory.
The Canadian team which managed to create a child from immature eggs was working with only around a dozen.
Another advantage is that the follicles mature much more quickly in the lab than they do in the ovary.
The scientists do not yet know whether eggs - or oocytes, to give them their technical name - matured in this way are completely normal and suitable for in-vitro fertilisation. But animal studies suggest they are.
The next step is to use hormones and other substances to try to nudge the 'antral' eggs on to the next stage of maturation, and then test the technique on humans.
"We believe there's good evidence that we can get normal oocytes, but of course you would never apply this technique clinically until you are sure," said Dr Telfer.
"We're seeking funding for further research to bridge that gap. It might take five to ten years from now before we get to the stage of a clinical trial."
Dr Jane Stewart, consultant in reproductive medicine at the Newcastle Fertility Centre, said:
"This work increases our understanding of the maturation of human eggs in the lab and takes us a step nearer the goal of strong immature eggs for fertility preservation for women."
Source: http://www.dailymail.co.uk/pages/live/articles/health/healthmain.html?in_article_id=560951&in_page_id=1774
Life Begins...
Miscarriage stories of loss, hope & help
http://born2luv.blogspot.com/
Stories of Pregnancy & Birth over 44y
- Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
4,600 Stories of Pregnancy & Birth over 44y
Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
 A major breakthrough by British scientists could bring new hope for women facing the heartbreak of infertility.
A major breakthrough by British scientists could bring new hope for women facing the heartbreak of infertility.For the first time a team has managed to grow hundreds of eggs in the laboratory using a new technique which could help cancer patients whose treatment can leave them infertile.
It would also allow thousands more women to wait until middle age to have children.
The scientists from Edinburgh University have shown that immature eggs can be frozen, grown and matured in the lab.
The process could lead to women having pieces of ovary containing the immature eggs removed and stored. Much later on, they could be thawed, fertilised and finally implanted into the womb.
The breakthrough, which comes as MPs prepare to debate the controversial Human Fertilisation and Embryology Bill, raises again the ethical debate surrounding the freezing of eggs.
Some say it is morally wrong for a woman to do so and have them fertilised years later in order to delay having children while she pursues a career.
However, scientists hope the new process will revolutionise fertility preservation for women because it will allow them to store many more eggs than they can under traditional IVF techniques.
And, because immature eggs survive the freezing process much better than the mature ones used in IVF, it is much more likely that older women will be able to conceive using them.
It brings forward the prospect that thousands of women will use the technique to side-step the menopause, delaying motherhood for the sake of their careers.
The process, which could be available in five years, also provides hope for cancer sufferers who at the moment are often left infertile following chemotherapy and radiotherapy.
Powerful anti-cancer drugs can destroy follicles in the ovaries, wiping out any possibility of women having children.
At the moment, these women have a piece of ovary removed, frozen and then re-transplanted after their cancer treatment. But there is always the danger that the cancer could be reintroduced by the implant.
The new technique means women's immature eggs contained in the patch of ovary could be grown in the lab and then screened for cancer before being used in IVF treatment.
There are also hopes it will provide a rich source of eggs for scientists to study for clues on ways to treat a range of diseases.
There is a shortage of human eggs for medical research, and if the technique works it would bypass the controversy over the use of animal-human 'hybrid' embryos.
The Human Fertilisation and Embryology Bill, which MPs are due to debate next month, would allow scientists to use these embryos in medical research, but many MPs plan to vote against.
The research, carried out by an Edinburgh University team led by Dr Evelyn Telfer, is published today in the journal Human Reproduction.
"This is a significant step in developing immature eggs to maturity outside the body," said Dr Telfer.
"Women who face infertility as a result of chemotherapy, or who want to put their biological clock on hold, could benefit from this system.
"However, there is a lot more research to be carried out before this technique could be safely applied within a clinical setting."
Last year, Canadian scientists announced the first birth of a child created from a human egg matured in the laboratory.
However, they did not use the same "primordial follicles" studied by the researchers from Edinburgh.
These are the tiny egg-bearing pockets within the ovaries that are present in their millions at birth, but gradually die off over the course of a woman's life.
They represent a woman's fertility "battery" which once depleted cannot be recharged.
Many remain dormant, but some go on to mature and eventually release their eggs in preparation for fertilisation.
For the first time, the team led by Dr Telfer has succeeded in growing primordial follicles to a late stage of maturation in the lab.
They took pieces of ovary containing the follicles from six volunteer women who were giving birth by caesarean section.
These were then exposed to a chemical that promotes growth, similar to the one that functions in the ovaries.
Around a third of them survived and went on to reach the advanced 'antral' stage of development.
At this stage, the follicles are filled with fluid and contain eggs almost ready to be fertilised.
It means that it could soon be possible to grow hundreds of eggs in the laboratory.
The Canadian team which managed to create a child from immature eggs was working with only around a dozen.
Another advantage is that the follicles mature much more quickly in the lab than they do in the ovary.
The scientists do not yet know whether eggs - or oocytes, to give them their technical name - matured in this way are completely normal and suitable for in-vitro fertilisation. But animal studies suggest they are.
The next step is to use hormones and other substances to try to nudge the 'antral' eggs on to the next stage of maturation, and then test the technique on humans.
"We believe there's good evidence that we can get normal oocytes, but of course you would never apply this technique clinically until you are sure," said Dr Telfer.
"We're seeking funding for further research to bridge that gap. It might take five to ten years from now before we get to the stage of a clinical trial."
Dr Jane Stewart, consultant in reproductive medicine at the Newcastle Fertility Centre, said:
"This work increases our understanding of the maturation of human eggs in the lab and takes us a step nearer the goal of strong immature eggs for fertility preservation for women."
Source: http://www.dailymail.co.uk/pages/live/articles/health/healthmain.html?in_article_id=560951&in_page_id=1774
Life Begins...
Miscarriage stories of loss, hope & help
http://born2luv.blogspot.com/
Stories of Pregnancy & Birth over 44y
- Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
4,600 Stories of Pregnancy & Birth over 44y
Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
Photo by nubuck
 Found this on FertilityFriend today:
Found this on FertilityFriend today:
In the final sample, there were 224 singletons, 135 twins, and 32 triplets. Baseline HCG concentrations were significantly higher for twins and triplets compared to singletons (P greater than 0.0001) and for triplets compared to twins (P greater than 0.0001). The patients were predominantly Caucasian and nulliparous, and had an average of 3.01 ± 0.86 (range 1–6) embryos replaced at the time of transfer. Linear regression analysis of the initial values of log (HCG) were significantly influenced by the number of gestational sacs (P greater than 0.0001) and maternal body mass index (BMI) (P = 0.01).
Life Begins...
Miscarriage stories of loss, hope & help
http://born2luv.blogspot.com/
Stories of Pregnancy & Birth over 44y
- Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
4,600 Stories of Pregnancy & Birth over 44y
Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
Recent Keyword Searches: fertility ovulation 40, am i too old to have a baby at 43, do women on the pill have more eggs later in life?, safe age group to get pregnant, is it possible to get pregnant at 50?, late life pregnancy trend, can a 40 yr old woman bear children, have women gotten pregnant in their 40's, if a woman is post menopausal can she get pregnant?, how to get pregnant after 40
 Found this on FertilityFriend today:
Found this on FertilityFriend today:Jennifer asked: A thought occurred to me last night while I was trying to go to sleep about beta numbers.
I am 5' 10" and a size 16.... My best friend is 5' 0" and a size "zero". Considering that a smaller person like my friend has a lower total blood volume than someone larger like myself wouldn't the concentration of hcg be different even if we happened to be the same dpo [days past ovulation] and pregnant? Wouldn't the concentration be stronger (higher beta #'s) in a smaller person than in a bigger person, since the concentration would be different because of the different amounts of total blood volume in our bodies?
Catherine posted the following research study:
Defining the rise of serum HCG in viable pregnancies achieved through use of IVF
In the final sample, there were 224 singletons, 135 twins, and 32 triplets. Baseline HCG concentrations were significantly higher for twins and triplets compared to singletons (P greater than 0.0001) and for triplets compared to twins (P greater than 0.0001). The patients were predominantly Caucasian and nulliparous, and had an average of 3.01 ± 0.86 (range 1–6) embryos replaced at the time of transfer. Linear regression analysis of the initial values of log (HCG) were significantly influenced by the number of gestational sacs (P greater than 0.0001) and maternal body mass index (BMI) (P = 0.01).
HCG levels were higher among twins and triplets compared to singletons, and lower among women with greater BMI. In the multivariable regression, there was no independent effect of number of embryos transferred, use of ICSI [intracytoplasmic sperm injection], or use of AH [Assisted hatching] on initial log (HCG) values. Infertility centre was also analysed as an independent variable and was found to have no significant effect.
We also observed that HCG concentrations were significantly lower among obese women (BMI greater than 30 kg/m2) compared to normal-weight women, but rates of increase were similar. Physiological mechanisms underlying this finding are speculative, but may be related to the fat tissue’s capacity to act as a steroid hormone reservoir and site of hormone metabolism (Deslypere et al., 1985).
Source: http://humrep.oxfordjournals.org/cgi/content/full/21/3/823
Source: http://humrep.oxfordjournals.org/cgi/content/full/21/3/823
Life Begins...
Miscarriage stories of loss, hope & help
http://born2luv.blogspot.com/
Stories of Pregnancy & Birth over 44y
- Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
4,600 Stories of Pregnancy & Birth over 44y
Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
Recent Keyword Searches: fertility ovulation 40, am i too old to have a baby at 43, do women on the pill have more eggs later in life?, safe age group to get pregnant, is it possible to get pregnant at 50?, late life pregnancy trend, can a 40 yr old woman bear children, have women gotten pregnant in their 40's, if a woman is post menopausal can she get pregnant?, how to get pregnant after 40
Photo by tlgoa
 More than six million American women and their partners face some kind of infertility issue. Fertility treatments like in vitro fertilization have helped millions, but what about women who still can't conceive?
More than six million American women and their partners face some kind of infertility issue. Fertility treatments like in vitro fertilization have helped millions, but what about women who still can't conceive?
In 1997, embryologist Michael Tucker became the first United States scientist to produce a baby from a frozen donor egg. Freezing eggs was groundbreaking technology then, but…
"The potential was as low as five percent per thawing that you would actually end up with a baby," says Michael Tucker, Ph.D., an embryologist with Georgia Reproductive Specialists in Atlanta. "These were not good odds."
Now Dr. Tucker says he's found a new process called that significantly improves the odds.
"By avoiding ice formation -- especially with the human egg, which is the largest cell in the human body -- we are able to get much more consistent survival of the cell," Dr. Tucker says.
Eggs are flash frozen in thin tubes, then thawed later for use. Dr. Tucker says 80 percent of eggs survive this process … compared to about 50-percent with conventional freezing. And that means better odds overall.
"That's what you want to be able to say to an individual woman, we can offer consistently a 30 percent chance per attempt of thawing your eggs using this process of actually having a live born baby," Dr. Tucker says.
After three years of unsuccessful fertility treatments, Kurena and Mark Hill became Dr. Tucker's first test case for vitrification. Now they have Rylie -- Dr. Tucker's newest success story. The new egg freezing technology is still experimental, and the idea itself is still controversial. But for the Hills, having their daughter means everything.
"Oh my God, she means … sorry to cry, but she means so much to me," Kurena says. "She's such my miracle."
It's too soon to say whether this new egg freezing technique can be an option for women in their 30's and 40's trying to save their eggs for the future. The American Society for Reproductive Medicine warns that egg freezing in general "should not be marketed or used as a means to defer reproductive aging."
FOR MORE INFORMATION, PLEASE CONTACT:
Georgia Reproductive Specialists
http://www.ivf.com
Source: http://www.news4jax.com/health/15943361/detail.html
Life Begins...
Miscarriage stories of loss, hope & help
http://born2luv.blogspot.com/
Stories of Pregnancy & Birth over 44y
- Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
4,600 Stories of Pregnancy & Birth over 44y
Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
 More than six million American women and their partners face some kind of infertility issue. Fertility treatments like in vitro fertilization have helped millions, but what about women who still can't conceive?
More than six million American women and their partners face some kind of infertility issue. Fertility treatments like in vitro fertilization have helped millions, but what about women who still can't conceive?In 1997, embryologist Michael Tucker became the first United States scientist to produce a baby from a frozen donor egg. Freezing eggs was groundbreaking technology then, but…
"The potential was as low as five percent per thawing that you would actually end up with a baby," says Michael Tucker, Ph.D., an embryologist with Georgia Reproductive Specialists in Atlanta. "These were not good odds."
Now Dr. Tucker says he's found a new process called that significantly improves the odds.
"By avoiding ice formation -- especially with the human egg, which is the largest cell in the human body -- we are able to get much more consistent survival of the cell," Dr. Tucker says.
Eggs are flash frozen in thin tubes, then thawed later for use. Dr. Tucker says 80 percent of eggs survive this process … compared to about 50-percent with conventional freezing. And that means better odds overall.
"That's what you want to be able to say to an individual woman, we can offer consistently a 30 percent chance per attempt of thawing your eggs using this process of actually having a live born baby," Dr. Tucker says.
After three years of unsuccessful fertility treatments, Kurena and Mark Hill became Dr. Tucker's first test case for vitrification. Now they have Rylie -- Dr. Tucker's newest success story. The new egg freezing technology is still experimental, and the idea itself is still controversial. But for the Hills, having their daughter means everything.
"Oh my God, she means … sorry to cry, but she means so much to me," Kurena says. "She's such my miracle."
It's too soon to say whether this new egg freezing technique can be an option for women in their 30's and 40's trying to save their eggs for the future. The American Society for Reproductive Medicine warns that egg freezing in general "should not be marketed or used as a means to defer reproductive aging."
FOR MORE INFORMATION, PLEASE CONTACT:
Georgia Reproductive Specialists
http://www.ivf.com
Source: http://www.news4jax.com/health/15943361/detail.html
Life Begins...
Miscarriage stories of loss, hope & help
http://born2luv.blogspot.com/
Stories of Pregnancy & Birth over 44y
- Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
4,600 Stories of Pregnancy & Birth over 44y
Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
Photo by stylesr1
 London, April 21 (ANI): Scot scientists have achieved a breakthrough in taking early stage follicles tiny egg-bearing pockets in the ovaries from a woman’s ovaries, and maturing them into eggs in the lab for the first time.
London, April 21 (ANI): Scot scientists have achieved a breakthrough in taking early stage follicles tiny egg-bearing pockets in the ovaries from a woman’s ovaries, and maturing them into eggs in the lab for the first time.
The achievement of Edinburgh University researchers means that women undergoing cancer treatment, or wishing to delay motherhood to concentrate on their careers, may have a way of preserving their fertility in the next five to 10 years.
Dr Evelyn Telfer and her colleagues say that they have established a procedure to develop early stage follicles to a much later stage.
The researchers took pieces of ovary containing the follicles from six volunteer women who were giving birth by elective caesarean section, and exposed them to an artificial growth factor.
They revealed that about one-third of the follicles survived, and went on to reach an advanced stage.
“This is a significant step in developing immature eggs to maturity outside the body. Women who face infertility as a result of chemotherapy, or who want to put their biological clock on hold, could benefit from this system, the Scotsman quoted Dr. Telfer as saying.
“However, there is a lot more research to be carried out before this technique could be safely applied within a clinical setting,” she added.
Normally, a woman undergoing cancer treatment has to have a piece of ovary removed and frozen for future transplantation, a procedure that carries the risk of reintroducing cancer cells to the patient.
They may also rely on fertility medication to produce eggs to be harvested for use at a later date, but this poses risks in delaying treatment, and defrosting the eggs does not always work.
Dr Telfer says that one alternative may be to maturing eggs in the laboratory may make it possible to screen them for cancer before they are returned.
In a report published in the journal Human Reproduction, the researcher says that women wishing to preserve their fertility past the menopause may also have their follicles stored for later use when they are ready to start a family.
She has revealed that in animal studies, eggs matured in this way appear to be completely normal and suitable for in vitro fertilisation.
However, her team have yet to confirm the same for humans.
“We believe there’s good evidence that we can get normal oocytes (eggs], but of course you would never apply this technique clinically until you are sure,” said Dr Telfer. (ANI)
Source: http://www.thaindian.com/newsportal/india-news/breakthrough-may-preserve-fertility-post-menopause_10040356.html
Life Begins...
Miscarriage stories of loss, hope & help
http://born2luv.blogspot.com/
Stories of Pregnancy & Birth over 44y
- Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
4,550 Stories of Pregnancy & Birth over 44y
Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
Recent Keyword Searches: fertility at 40, soft ivf, in vitro donor egg forty, 34 and pregnant is that too old?, normal periods over 44 can i get pregnant, should i go abroad for doner eggs to get pregnant at 42, how to get pregnant after age 40, can a 51 year old woman get pregnant, best way to get pregnant at the age of 40, natural ways to get pregnant at 40
 London, April 21 (ANI): Scot scientists have achieved a breakthrough in taking early stage follicles tiny egg-bearing pockets in the ovaries from a woman’s ovaries, and maturing them into eggs in the lab for the first time.
London, April 21 (ANI): Scot scientists have achieved a breakthrough in taking early stage follicles tiny egg-bearing pockets in the ovaries from a woman’s ovaries, and maturing them into eggs in the lab for the first time.The achievement of Edinburgh University researchers means that women undergoing cancer treatment, or wishing to delay motherhood to concentrate on their careers, may have a way of preserving their fertility in the next five to 10 years.
Dr Evelyn Telfer and her colleagues say that they have established a procedure to develop early stage follicles to a much later stage.
The researchers took pieces of ovary containing the follicles from six volunteer women who were giving birth by elective caesarean section, and exposed them to an artificial growth factor.
They revealed that about one-third of the follicles survived, and went on to reach an advanced stage.
“This is a significant step in developing immature eggs to maturity outside the body. Women who face infertility as a result of chemotherapy, or who want to put their biological clock on hold, could benefit from this system, the Scotsman quoted Dr. Telfer as saying.
“However, there is a lot more research to be carried out before this technique could be safely applied within a clinical setting,” she added.
Normally, a woman undergoing cancer treatment has to have a piece of ovary removed and frozen for future transplantation, a procedure that carries the risk of reintroducing cancer cells to the patient.
They may also rely on fertility medication to produce eggs to be harvested for use at a later date, but this poses risks in delaying treatment, and defrosting the eggs does not always work.
Dr Telfer says that one alternative may be to maturing eggs in the laboratory may make it possible to screen them for cancer before they are returned.
In a report published in the journal Human Reproduction, the researcher says that women wishing to preserve their fertility past the menopause may also have their follicles stored for later use when they are ready to start a family.
She has revealed that in animal studies, eggs matured in this way appear to be completely normal and suitable for in vitro fertilisation.
However, her team have yet to confirm the same for humans.
“We believe there’s good evidence that we can get normal oocytes (eggs], but of course you would never apply this technique clinically until you are sure,” said Dr Telfer. (ANI)
Source: http://www.thaindian.com/newsportal/india-news/breakthrough-may-preserve-fertility-post-menopause_10040356.html
Life Begins...
Miscarriage stories of loss, hope & help
http://born2luv.blogspot.com/
Stories of Pregnancy & Birth over 44y
- Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
4,550 Stories of Pregnancy & Birth over 44y
Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
Recent Keyword Searches: fertility at 40, soft ivf, in vitro donor egg forty, 34 and pregnant is that too old?, normal periods over 44 can i get pregnant, should i go abroad for doner eggs to get pregnant at 42, how to get pregnant after age 40, can a 51 year old woman get pregnant, best way to get pregnant at the age of 40, natural ways to get pregnant at 40
Photo by http://www.mirror.co.uk/
+and+Siobhan.jpg) After years of using more and more drugs to boost fertility, doctors have found a new way to help women have babies... by going back to basics
After years of using more and more drugs to boost fertility, doctors have found a new way to help women have babies... by going back to basics
TODAY'S BOOK SUGGESTION:

 Murphy Lives Here
Murphy Lives Here
by Dr. Merryl J. Polak
-- Initially apprehensive about becoming a mother, Emma mapped out her life plans steered by fulfillment of a happy marriage and career.
She thought she might one day feel ready and willing to add the role of mother to her life's responsibilities, but she had not quite figured out when that would occur.
When Emma's biological clock smacked her upside the head and she suddenly craved motherhood over every other aspect of life, she was stunned to discover that she could not get pregnant.
After a year of ovulation test kits and timed baby making under her belt, it was inevitable that other avenues needed exploration.
After pursuing every option, including adoption, Emma learned that becoming a parent was not as simple a process as she had always envisioned.
 Paperback: 226 pages
Paperback: 226 pages
Click to order/for more info: Murphy Lives Here
 Start reading Murphy Lives Here on your Kindle in under a minute!
Start reading Murphy Lives Here on your Kindle in under a minute!
Don't have a Kindle? Get your Kindle here, or download a FREE Kindle Reading App.
+and+Siobhan.jpg) After years of using more and more drugs to boost fertility, doctors have found a new way to help women have babies... by going back to basics
After years of using more and more drugs to boost fertility, doctors have found a new way to help women have babies... by going back to basics
Every year, thousands of women suffer terrible physical side-effects and heartbreak as they go through gruelling IVF in their desperation to become mums.
But now, a revolutionary new form of IVF could make their dreams come true without the suffering and at a fraction of the cost.
The technique - Soft IVF - uses fewer drugs, significantly reducing the side-effects which the hormone injections in conventional treatment often cause.
It is also around half the price of the standard approach - about £2,000 compared to at least £4,000.
This month, at a fertility conference in London, doctors agreed Soft IVF was the future in fertility medicine.
They said the treatment - also known as Mild IVF - has good success rates and is safer for women because it interferes less with their body's natural chemistry.
Professor Bart Fauser, head of Reproductive Medicine in Utrecht, The Netherlands, has been recommending it over conventional IVF for the past three years.
"The evidence is that a mild approach significantly reduces the risks and side-effects," he says.
Dr Geeta Nargund, Head of Reproductive Medicine at St George's Hospital, London, and Medical Director of Create Health Clinic, is one of a handful of UK doctors offering. the new treatment.
She says: "It's safer for women to use no drugs or fewer drugs to achieve a pregnancy. It is safer for her own health, her eggs and any embryos that are created."
Any woman recommended for IVF can use it - from those with blocked fallopian tubes, to couples with unexplained infertility or those whose partners who have low-quality sperm.
Older women particularly benefit because their ovaries do not respond well to high drug stimulation.
So why is it different?
Conventional IVF relies on a woman injecting hormones for around four weeks, first to shut down her monthly cycle and next, to stimulate her ovaries to produce several eggs rather than the usual one.
These are later removed and mixed with sperm, in the hope that they will be fertilised. Once fertilised, the embryo is inserted into her womb, where it will hopefully attach to the lining and develop into a baby.
Soft IVF completely skips the first stage. Women begin by taking tiny quantities of hormones for up to a week to gently support egg production before following the rest of the steps in the same way.
How successful is it?
With one in six British couples suffering infertility, and a growing number opting for IVF each year, the new approach could mean good news for tens of thousands of couples.
Latest figures point to an average success rate of 27 per cent for IVF in the UK.
In a follow-up study published last year, scientists in The Netherlands found a 43 per cent success rate for women using Soft IVF.
It is also possible to opt for drug-free or natural IVF, a technique which is particularly good for older women and even cheaper (around £1,000).
However, success rates are around 10 per cent per cycle, so several attempts are often necessary.
The side-effects
Women who undergo soft and natural IVF report few or no side-effects.
Dr Nargund says: "The single most serious complication of IVF cycles is ovarian hyperstimulation syndrome, which can be avoided by natural cycle and mild IVF."
Doctors have also discovered that using fewer drugs is safer for any developing babies. Scientists in Spain recently reported that stimulatory drugs affect the quality of the lining of the womb and even increases the chance of miscarriage.
Dr Nargund says: "If you can have a healthy baby and reduce the risk to your own health by using fewer drugs and spending less money then why would you want to spend more money to take more drugs?"
WHAT ARE YOUR OPTIONS?
Standard IVF
A woman begins by injecting a course of artificial hormones, which can bring on menopause-like symptoms. Next, she begins daily hormone injections for between three and four weeks to stimulate egg production.
Ten-12 days later, when her eggs are mature, as many as 20-30 are removed in a surgical procedure and mixed with the sperm. If successfully fertilised, two embryos are returned to her womb in the hope that at least one will develop into a baby.
'Soft' and 'natural' IVF techniques
The soft option misses out the first stage and, on days 3-7 of her period, she takes very small quantities of hormones to support her own natural egg production. Typically, around two to seven eggs are produced. She then follows the same process as before. Natural IVF misses the first two stages and no stimulatory drugs are used.
New breakthrough
A new technique could bring hope to women facing infertility.
Scottish scientists have found a way of taking pieces of ovary containing immature eggs and maturing them in a lab.
Immature eggs survive the freezing process much better but more research needs to be done to confirm it they're completely normal and suitable for IVF. If successful, it would benefit women who want to wait until they're older to have children or those who have had cancer treatment.
REAL LIFE SUCCESS STORIES
"I didn't want to blast my body with drugs"
Dr Marina Murphy, 40, and her husband Rory had Radha, now nine months old, after using natural IVF.
Rory and I had been trying to start a family for three years with no luck. When I hit 38, I started to panic and went to see my GP. Tests confirmed I had premature ovarian failure. I was told that my ovaries may no longer be producing eggs.
It meant I didn't have time to waste. I went on the NHS waiting list but I knew I couldn't rely on that (That was two-and-a-half years ago and I'm still waiting for an appointment!).
I chose a private clinic called Create Health. The more I heard about natural and Soft IVF, the more I liked the sound of them.
As a chemist, I understand the need for drugs but I also believe it's better if you can avoid taking them. I didn't want to blast my body with huge doses of drugs. I like a more gentle approach.
I also liked being able to go on to do another cycle if the previous one failed, which you can't with conventional IVF.
It is more physically demanding so, if it doesn't work, you need a break. I preferred the idea of moving on to the next treatment as soon as possible.
Natural IVF turned out to be very straightforward. I had no side-effects and wasn't stressed by the process. We never assumed that IVF would work but it was amazing when it did - on our third attempt.
Now we have Radha, a beautiful boy who has transformed our lives.
"I immediately knew Soft IVF was for me"
Siobhan McLernon, 40, and her 43-year-old fiance Shaun opted for Soft IVF and were rewarded with daughter Cara-Mae.
Being told I had blocked fallopian tubes was a shock. It meant my eggs couldn't reach my womb, so it was impossible for me to get pregnant naturally. I was told we'd need IVF.
It took months to get a referral to an NHS fertility specialist and when I did, I was told it would be around two years before I could start treatment.
It was time we didn't have, so Shaun and I decided we had no choice but to pay.
The minute I heard about Soft IVF, I knew it was right for me. I did not want to pump myself full of hormones and we also couldn't afford the £8,000 some clinics charge - so Soft IVF felt like a lifeline.
The process was simple. After some blood tests to check my hormone levels, I began a seven-day course of injections and didn't experience any side-effects.
The hardest part was waiting two weeks to find out whether it had worked. In that time, I went through 100 emotions.
By the second week, I was convinced it hadn't worked. So when the pregnancy test said positive, I couldn't believe it! I was just the happiest person.
Every day, Cara-Mae brings us so much joy - I just can't imagine our life without her. She is such an amazing gift.
I would definitely recommend Soft IVF. If we had chosen a more expensive option we would have been under more pressure and it would have been more stressful.
Source: http://www.mirror.co.uk/showbiz/yourlife/2008/04/22/a-new-form-of-cheaper-more-natural-ivf-that-could-beat-infertility-and-make-you-a-mum-89520-20391376/
But now, a revolutionary new form of IVF could make their dreams come true without the suffering and at a fraction of the cost.
The technique - Soft IVF - uses fewer drugs, significantly reducing the side-effects which the hormone injections in conventional treatment often cause.
It is also around half the price of the standard approach - about £2,000 compared to at least £4,000.
This month, at a fertility conference in London, doctors agreed Soft IVF was the future in fertility medicine.
They said the treatment - also known as Mild IVF - has good success rates and is safer for women because it interferes less with their body's natural chemistry.
Professor Bart Fauser, head of Reproductive Medicine in Utrecht, The Netherlands, has been recommending it over conventional IVF for the past three years.
"The evidence is that a mild approach significantly reduces the risks and side-effects," he says.
Dr Geeta Nargund, Head of Reproductive Medicine at St George's Hospital, London, and Medical Director of Create Health Clinic, is one of a handful of UK doctors offering. the new treatment.
She says: "It's safer for women to use no drugs or fewer drugs to achieve a pregnancy. It is safer for her own health, her eggs and any embryos that are created."
Any woman recommended for IVF can use it - from those with blocked fallopian tubes, to couples with unexplained infertility or those whose partners who have low-quality sperm.
Older women particularly benefit because their ovaries do not respond well to high drug stimulation.
So why is it different?
Conventional IVF relies on a woman injecting hormones for around four weeks, first to shut down her monthly cycle and next, to stimulate her ovaries to produce several eggs rather than the usual one.
These are later removed and mixed with sperm, in the hope that they will be fertilised. Once fertilised, the embryo is inserted into her womb, where it will hopefully attach to the lining and develop into a baby.
Soft IVF completely skips the first stage. Women begin by taking tiny quantities of hormones for up to a week to gently support egg production before following the rest of the steps in the same way.
How successful is it?
With one in six British couples suffering infertility, and a growing number opting for IVF each year, the new approach could mean good news for tens of thousands of couples.
Latest figures point to an average success rate of 27 per cent for IVF in the UK.
In a follow-up study published last year, scientists in The Netherlands found a 43 per cent success rate for women using Soft IVF.
It is also possible to opt for drug-free or natural IVF, a technique which is particularly good for older women and even cheaper (around £1,000).
However, success rates are around 10 per cent per cycle, so several attempts are often necessary.
The side-effects
Women who undergo soft and natural IVF report few or no side-effects.
Dr Nargund says: "The single most serious complication of IVF cycles is ovarian hyperstimulation syndrome, which can be avoided by natural cycle and mild IVF."
Doctors have also discovered that using fewer drugs is safer for any developing babies. Scientists in Spain recently reported that stimulatory drugs affect the quality of the lining of the womb and even increases the chance of miscarriage.
Dr Nargund says: "If you can have a healthy baby and reduce the risk to your own health by using fewer drugs and spending less money then why would you want to spend more money to take more drugs?"
WHAT ARE YOUR OPTIONS?
Standard IVF
A woman begins by injecting a course of artificial hormones, which can bring on menopause-like symptoms. Next, she begins daily hormone injections for between three and four weeks to stimulate egg production.
Ten-12 days later, when her eggs are mature, as many as 20-30 are removed in a surgical procedure and mixed with the sperm. If successfully fertilised, two embryos are returned to her womb in the hope that at least one will develop into a baby.
'Soft' and 'natural' IVF techniques
The soft option misses out the first stage and, on days 3-7 of her period, she takes very small quantities of hormones to support her own natural egg production. Typically, around two to seven eggs are produced. She then follows the same process as before. Natural IVF misses the first two stages and no stimulatory drugs are used.
New breakthrough
A new technique could bring hope to women facing infertility.
Scottish scientists have found a way of taking pieces of ovary containing immature eggs and maturing them in a lab.
Immature eggs survive the freezing process much better but more research needs to be done to confirm it they're completely normal and suitable for IVF. If successful, it would benefit women who want to wait until they're older to have children or those who have had cancer treatment.
REAL LIFE SUCCESS STORIES
"I didn't want to blast my body with drugs"
Dr Marina Murphy, 40, and her husband Rory had Radha, now nine months old, after using natural IVF.
Rory and I had been trying to start a family for three years with no luck. When I hit 38, I started to panic and went to see my GP. Tests confirmed I had premature ovarian failure. I was told that my ovaries may no longer be producing eggs.
It meant I didn't have time to waste. I went on the NHS waiting list but I knew I couldn't rely on that (That was two-and-a-half years ago and I'm still waiting for an appointment!).
I chose a private clinic called Create Health. The more I heard about natural and Soft IVF, the more I liked the sound of them.
As a chemist, I understand the need for drugs but I also believe it's better if you can avoid taking them. I didn't want to blast my body with huge doses of drugs. I like a more gentle approach.
I also liked being able to go on to do another cycle if the previous one failed, which you can't with conventional IVF.
It is more physically demanding so, if it doesn't work, you need a break. I preferred the idea of moving on to the next treatment as soon as possible.
Natural IVF turned out to be very straightforward. I had no side-effects and wasn't stressed by the process. We never assumed that IVF would work but it was amazing when it did - on our third attempt.
Now we have Radha, a beautiful boy who has transformed our lives.
"I immediately knew Soft IVF was for me"
Siobhan McLernon, 40, and her 43-year-old fiance Shaun opted for Soft IVF and were rewarded with daughter Cara-Mae.
Being told I had blocked fallopian tubes was a shock. It meant my eggs couldn't reach my womb, so it was impossible for me to get pregnant naturally. I was told we'd need IVF.
It took months to get a referral to an NHS fertility specialist and when I did, I was told it would be around two years before I could start treatment.
It was time we didn't have, so Shaun and I decided we had no choice but to pay.
The minute I heard about Soft IVF, I knew it was right for me. I did not want to pump myself full of hormones and we also couldn't afford the £8,000 some clinics charge - so Soft IVF felt like a lifeline.
The process was simple. After some blood tests to check my hormone levels, I began a seven-day course of injections and didn't experience any side-effects.
The hardest part was waiting two weeks to find out whether it had worked. In that time, I went through 100 emotions.
By the second week, I was convinced it hadn't worked. So when the pregnancy test said positive, I couldn't believe it! I was just the happiest person.
Every day, Cara-Mae brings us so much joy - I just can't imagine our life without her. She is such an amazing gift.
I would definitely recommend Soft IVF. If we had chosen a more expensive option we would have been under more pressure and it would have been more stressful.
Source: http://www.mirror.co.uk/showbiz/yourlife/2008/04/22/a-new-form-of-cheaper-more-natural-ivf-that-could-beat-infertility-and-make-you-a-mum-89520-20391376/
TODAY'S BOOK SUGGESTION:

by Dr. Merryl J. Polak
-- Initially apprehensive about becoming a mother, Emma mapped out her life plans steered by fulfillment of a happy marriage and career.
She thought she might one day feel ready and willing to add the role of mother to her life's responsibilities, but she had not quite figured out when that would occur.
When Emma's biological clock smacked her upside the head and she suddenly craved motherhood over every other aspect of life, she was stunned to discover that she could not get pregnant.
After a year of ovulation test kits and timed baby making under her belt, it was inevitable that other avenues needed exploration.
After pursuing every option, including adoption, Emma learned that becoming a parent was not as simple a process as she had always envisioned.
Click to order/for more info: Murphy Lives Here
Don't have a Kindle? Get your Kindle here, or download a FREE Kindle Reading App.
Photo by http://www.jstandard.com/
 Speaking as an older mother in a very young Jewish community of 20- and 30-something parents, I find myself much outside of the box. It is not exactly by choice that I have a late-in-life child. Some things simply happen, and others are meant to be in a way that is indefinable. Parenting is a tough job with a partner and support system, and 100 times harder flying solo.
Speaking as an older mother in a very young Jewish community of 20- and 30-something parents, I find myself much outside of the box. It is not exactly by choice that I have a late-in-life child. Some things simply happen, and others are meant to be in a way that is indefinable. Parenting is a tough job with a partner and support system, and 100 times harder flying solo.
I had already raised three children to emancipation and lost my life partner when a situation arose that led me to motherhood yet again. It was an unusual occurrence and like many women in their 40's, I had long stopped actively thinking of babies and caring for them. Or perhaps not, for the year that my husband died I had the opportunity to adopt yet another infant. I did not give it much thought, for the decision had already been made by some unfulfilled mothering instincts that were still inside my heart. I was reaching the end of my 40's when I adopted my son, the age at which my neighbors were already grand-parenting or at least, paying off college tuitions.
Of course, being a divorced mother is far from unusual in the suburbs, but being an adoptive single mother at my age certainly was. From the start, it was all-consuming and very tedious caring for a young infant. I had little time to think about my situation, but simply went with it, relearning all I had forgotten about infants as well as re-buying what I had long, long ago thrown out. Sleepless nights with a sick child are not fun for the best of us, least of all for me. I also had to rethink my position among my contemporaries, finding that many of my so-called friends were not terribly interested in my new baby and his day to day progress. I was knee-deep in dirty diapers, finger foods, "Goodnight Moon," SpongeBob, Legos, and local parks, where I found myself spending a good few hours each day. Admittedly, it bored me to tears, especially when I found that the younger mothers thought I was his grandmother and for the most part ignored my presence. I found my place by starting conversations on child development, preschools, and babysitters with those who deigned to acknowledge me as one of them.
I loved and adored my son beyond all else. He was the center of my universe, and this time there were no other children to compete for my attention. I worked part-time in the first few years and kept money coming in as well as remaining a part of the adult world. Coming home to a young child was lonely, and I often missed the companionship of men and women my age, who disappeared almost as quickly as they appeared in my life, easily tiring of the noise, commotion, and attention I gave mostly to this beautiful child.
As he grew, it did become easier for me. A precocious child, he loved to talk both at home and to other adults, finding himself the center of everyone’s attention. So it often is with "only children." With all of the issues involved and the loss of my own mother, focusing on my son became the way of life I chose.
I had another chance at loving and raising a child and being a "do-it-yourself" grandma for the first time, all at once. Isolation from my contemporaries was an issue, but over the years I have met several other older moms, perhaps in different life situations, to whom I could talk about something other than school and play dates. Fortunately I have made some friends of other adoptive moms, who understand exactly where I come from. We live in our world of work, and then our unique and difficult world of raising a child alone, with just a little less koach than those at the parent-teacher meetings.
I will be an active, 24/7 mother long after others have forgotten what that is like, but so what? I believe that women should have a choice as to when they should have children. Technology is changing and giving women more time in which to bear children. As we tend to live longer than men anyway, it should be our right and privilege to do so.
Adoption is a beautiful way to become a mother, and those older children in foster care, who are no longer "desirable" because of their ages, handicaps, or cultural backgrounds, would do well with a parent who was devoted and loving regardless of his or her chronological age.
My home is no longer as neat and clean as it was pre-last child, nor do I always feel relaxed with contemporaries, as my mind is elsewhere. Others of my age might begin to be forgetful, but I am not permitted to forget. I cannot imagine what disasters would befall us if I did. I am certainly driving more carefully and not taking risks I might have taken before or even now, without a growing child. I am reluctant to have guests in my home, as nothing is new or in place the way I would like it to be, and I am more careful with money because of the expense of childrearing. There are no grandparents as other children might have with whom to celebrate the myriad of Jewish holidays or to give my son gifts, and often it is saddening. When I think of his bar mitzvah coming this year, my heart sinks at the thought that now he has no father or grandfather to stand with him, and no grandmothers to sit with me and kvell. Yet no one’s life is perfect.
I enjoy so much about being a mother to my son and watching his clothes shrink as he grows. I have more time and understanding for him than I did for my other three children, two of whom are now parents as well, but I do repeat mistakes, and often my patience wears dangerously thin. What a fallacy that we are more patient. There are so many things I have learned from my experience and I must often stand by and hold my tongue seeing my now younger friends and neighbors make foolish mistakes because they have "read something in a book."
I probably could write the longest-ever "book of mistakes" myself, but I just do the best I can. I am so full of love for my child, and all that is returned to me as my son grows up and, finally, just maybe, so do I.
Source: http://www.jstandard.com/articles/3941/1/A-somewhat-older-mom-speaks-out
Life Begins...
Miscarriage stories of loss, hope & help
http://born2luv.blogspot.com/
Stories of Pregnancy & Birth over 44y
- Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
4,550 Stories of Pregnancy & Birth over 44y
Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
Recent Keyword Searches: over 40 pregnancy success, is 44 years old too old to be fertile, having a baby 40s, i am pregnant at age 45 is it safe, at age 50 how likely is a woman to get pregnant, can i get pregnant at 40, can you still get pregnant if you going through menopause, pre menopause can get pregnant?, women over 45 natural pregnancy, oldest woman in united states to get pregnant or have a baby
 Speaking as an older mother in a very young Jewish community of 20- and 30-something parents, I find myself much outside of the box. It is not exactly by choice that I have a late-in-life child. Some things simply happen, and others are meant to be in a way that is indefinable. Parenting is a tough job with a partner and support system, and 100 times harder flying solo.
Speaking as an older mother in a very young Jewish community of 20- and 30-something parents, I find myself much outside of the box. It is not exactly by choice that I have a late-in-life child. Some things simply happen, and others are meant to be in a way that is indefinable. Parenting is a tough job with a partner and support system, and 100 times harder flying solo.I had already raised three children to emancipation and lost my life partner when a situation arose that led me to motherhood yet again. It was an unusual occurrence and like many women in their 40's, I had long stopped actively thinking of babies and caring for them. Or perhaps not, for the year that my husband died I had the opportunity to adopt yet another infant. I did not give it much thought, for the decision had already been made by some unfulfilled mothering instincts that were still inside my heart. I was reaching the end of my 40's when I adopted my son, the age at which my neighbors were already grand-parenting or at least, paying off college tuitions.
Of course, being a divorced mother is far from unusual in the suburbs, but being an adoptive single mother at my age certainly was. From the start, it was all-consuming and very tedious caring for a young infant. I had little time to think about my situation, but simply went with it, relearning all I had forgotten about infants as well as re-buying what I had long, long ago thrown out. Sleepless nights with a sick child are not fun for the best of us, least of all for me. I also had to rethink my position among my contemporaries, finding that many of my so-called friends were not terribly interested in my new baby and his day to day progress. I was knee-deep in dirty diapers, finger foods, "Goodnight Moon," SpongeBob, Legos, and local parks, where I found myself spending a good few hours each day. Admittedly, it bored me to tears, especially when I found that the younger mothers thought I was his grandmother and for the most part ignored my presence. I found my place by starting conversations on child development, preschools, and babysitters with those who deigned to acknowledge me as one of them.
I loved and adored my son beyond all else. He was the center of my universe, and this time there were no other children to compete for my attention. I worked part-time in the first few years and kept money coming in as well as remaining a part of the adult world. Coming home to a young child was lonely, and I often missed the companionship of men and women my age, who disappeared almost as quickly as they appeared in my life, easily tiring of the noise, commotion, and attention I gave mostly to this beautiful child.
As he grew, it did become easier for me. A precocious child, he loved to talk both at home and to other adults, finding himself the center of everyone’s attention. So it often is with "only children." With all of the issues involved and the loss of my own mother, focusing on my son became the way of life I chose.
I had another chance at loving and raising a child and being a "do-it-yourself" grandma for the first time, all at once. Isolation from my contemporaries was an issue, but over the years I have met several other older moms, perhaps in different life situations, to whom I could talk about something other than school and play dates. Fortunately I have made some friends of other adoptive moms, who understand exactly where I come from. We live in our world of work, and then our unique and difficult world of raising a child alone, with just a little less koach than those at the parent-teacher meetings.
I will be an active, 24/7 mother long after others have forgotten what that is like, but so what? I believe that women should have a choice as to when they should have children. Technology is changing and giving women more time in which to bear children. As we tend to live longer than men anyway, it should be our right and privilege to do so.
Adoption is a beautiful way to become a mother, and those older children in foster care, who are no longer "desirable" because of their ages, handicaps, or cultural backgrounds, would do well with a parent who was devoted and loving regardless of his or her chronological age.
My home is no longer as neat and clean as it was pre-last child, nor do I always feel relaxed with contemporaries, as my mind is elsewhere. Others of my age might begin to be forgetful, but I am not permitted to forget. I cannot imagine what disasters would befall us if I did. I am certainly driving more carefully and not taking risks I might have taken before or even now, without a growing child. I am reluctant to have guests in my home, as nothing is new or in place the way I would like it to be, and I am more careful with money because of the expense of childrearing. There are no grandparents as other children might have with whom to celebrate the myriad of Jewish holidays or to give my son gifts, and often it is saddening. When I think of his bar mitzvah coming this year, my heart sinks at the thought that now he has no father or grandfather to stand with him, and no grandmothers to sit with me and kvell. Yet no one’s life is perfect.
I enjoy so much about being a mother to my son and watching his clothes shrink as he grows. I have more time and understanding for him than I did for my other three children, two of whom are now parents as well, but I do repeat mistakes, and often my patience wears dangerously thin. What a fallacy that we are more patient. There are so many things I have learned from my experience and I must often stand by and hold my tongue seeing my now younger friends and neighbors make foolish mistakes because they have "read something in a book."
I probably could write the longest-ever "book of mistakes" myself, but I just do the best I can. I am so full of love for my child, and all that is returned to me as my son grows up and, finally, just maybe, so do I.
Source: http://www.jstandard.com/articles/3941/1/A-somewhat-older-mom-speaks-out
Life Begins...
Miscarriage stories of loss, hope & help
http://born2luv.blogspot.com/
Stories of Pregnancy & Birth over 44y
- Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
4,550 Stories of Pregnancy & Birth over 44y
Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
Recent Keyword Searches: over 40 pregnancy success, is 44 years old too old to be fertile, having a baby 40s, i am pregnant at age 45 is it safe, at age 50 how likely is a woman to get pregnant, can i get pregnant at 40, can you still get pregnant if you going through menopause, pre menopause can get pregnant?, women over 45 natural pregnancy, oldest woman in united states to get pregnant or have a baby
Photo by jaylopez
 Reproductive Assistance, the Midwest's premier full service egg donor, surrogate, and gestational carrier agency, awards needy family a free egg donor cycle.
Reproductive Assistance, the Midwest's premier full service egg donor, surrogate, and gestational carrier agency, awards needy family a free egg donor cycle.
The Get a Free Egg Donor contest that begun on January 1 ended March 31, 2008. Hundreds of families from all over the world entered and submitted online applications. The winning family was selected and won a free egg donor cycle, a $4,500 value.
Frances and Wesley, last name is not shared to remain anonymous, are from the Midwest. They are the first recipients of RAI's Get a Free Egg Donor cycle. Like most couples, they have had their share of heartache.
For the past seven years, Frances and Wesley have been trying to have a baby. They have seen four different fertility doctors in two different states. They have completed three artificial insemination cycles, four IVF cycles, three egg donors cycles, and suffered one miscarriage. Frances is quoted as saying, "It has been emotionally and financially draining. I was pregnant once and had a miscarriage after six weeks. It was the best six weeks of my life. But, I wonder if it was a curse. Our dream of having a child has been put to the test and receiving a free egg donor at this point of our journey would be a God send!"
Lisa Henkel, President and Owner of RAI, said, "Our company has helped thousands of families across the world create their families thru egg donors, surrogates, and gestational carriers. From the very beginning, the company took off and has grown every year. It is now time to give back to those families that are experiencing the challenges of infertility."
All of our donors, surrogates, and gestational carriers go through a rigorous application and screening process. Our agency is registered and follows ASRM guidelines.
Source: http://www.emaxhealth.com/4/21767.html
Life Begins...
Miscarriage stories of loss, hope & help
http://born2luv.blogspot.com/
Stories of Pregnancy & Birth over 44y
- Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
4,550 Stories of Pregnancy & Birth over 44y
Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
Recent Keyword Searches: postponing childbirth 40's career, what to ask your ob-gyn when trying to get pregnant, oldest that woman can get pregnant, can i get pregnant at 39, late ovulation perimenopause, can periods become more frequent at early stages of menopause, change of life babies, chances of prenancy over 40 years, having a child in your forties, is a fsh level of 14 too high to get pregnant
 Reproductive Assistance, the Midwest's premier full service egg donor, surrogate, and gestational carrier agency, awards needy family a free egg donor cycle.
Reproductive Assistance, the Midwest's premier full service egg donor, surrogate, and gestational carrier agency, awards needy family a free egg donor cycle.The Get a Free Egg Donor contest that begun on January 1 ended March 31, 2008. Hundreds of families from all over the world entered and submitted online applications. The winning family was selected and won a free egg donor cycle, a $4,500 value.
Frances and Wesley, last name is not shared to remain anonymous, are from the Midwest. They are the first recipients of RAI's Get a Free Egg Donor cycle. Like most couples, they have had their share of heartache.
For the past seven years, Frances and Wesley have been trying to have a baby. They have seen four different fertility doctors in two different states. They have completed three artificial insemination cycles, four IVF cycles, three egg donors cycles, and suffered one miscarriage. Frances is quoted as saying, "It has been emotionally and financially draining. I was pregnant once and had a miscarriage after six weeks. It was the best six weeks of my life. But, I wonder if it was a curse. Our dream of having a child has been put to the test and receiving a free egg donor at this point of our journey would be a God send!"
Lisa Henkel, President and Owner of RAI, said, "Our company has helped thousands of families across the world create their families thru egg donors, surrogates, and gestational carriers. From the very beginning, the company took off and has grown every year. It is now time to give back to those families that are experiencing the challenges of infertility."
All of our donors, surrogates, and gestational carriers go through a rigorous application and screening process. Our agency is registered and follows ASRM guidelines.
Source: http://www.emaxhealth.com/4/21767.html
Life Begins...
Miscarriage stories of loss, hope & help
http://born2luv.blogspot.com/
Stories of Pregnancy & Birth over 44y
- Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
4,550 Stories of Pregnancy & Birth over 44y
Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
Recent Keyword Searches: postponing childbirth 40's career, what to ask your ob-gyn when trying to get pregnant, oldest that woman can get pregnant, can i get pregnant at 39, late ovulation perimenopause, can periods become more frequent at early stages of menopause, change of life babies, chances of prenancy over 40 years, having a child in your forties, is a fsh level of 14 too high to get pregnant

A doctor is silhouetted as he walks past a poster showing images of the development of a human fetus at a fertility clinic.
In Brief:
5 Despite continuing refinements in fertility treatments, researchers have not been able to provide what career-minded adults seek: an extension of the years in which a woman is fertile.
5 The viability of conventionally frozen eggs is still inferior to that of frozen sperm and embryos.
5 The freezing of ovarian tissue, still highly experimental, may offer new options to cancer patients facing sterilizing treatments.
With genetic abnormalities in many embryos correcting themselves by day five, clinics are waiting longer to transfer embryos into patients.
In the nearly 30 years since Louise Brown made history as the first test-tube baby, more than one million infants have been conceived by means of in vitro fertilization. Assisted reproductive technologies continue to advance, but increasingly they are pushing against one of nature’s great barriers to fertility: maternal age.
“Many infertility specialists are surprised by the number of otherwise highly educated older couples with unrealistic expectations of fertility,” Dr. Bradley J. Van Voorhis, a fertility expert at the University of Iowa School of Medicine, wrote recently in The New England Journal of Medicine. “The negative effect of a woman’s age on fertility cannot be overemphasized.”
Certainly, new options to extend fertility are testing the limits of who can get pregnant, and when. They are also raising fresh medical, economic and ethical concerns.
Whereas scientists for decades have been freezing human embryos for later implantation into the womb, now a process called vitrification enables technicians to flash-freeze unfertilized human eggs in a matter of seconds, greatly improving their survival rates.
The process is considered superior to conventional slow-freezing methods because it prevents the formation of ice crystals in the egg that could damage DNA. Sperm later meets thawed egg through in vitro fertilization, and the resulting embryo is implanted in the womb. The technique increases the chances of successful pregnancy later in life for a young woman without a partner who must, or wants to, defer starting a family.
“I think this will emancipate women as much as the birth control pill did in 1960,” said Dr. Sherman Silber, a fertility specialist in St. Louis, Mo., one of a limited number of doctors in the country to offer the novel procedure. In a recent study in Spain, there were no differences in pregnancy rates in women undergoing in vitro fertilization with embryos from either fresh or flash-frozen eggs. About 45 percent in each group conceived.
The experimental procedure, however, is not without its sacrifices — and skeptics. Potent drugs must be used to stimulate a patient’s ovaries, and then the eggs must be aspirated while she is sedated. Vitrification is also expensive, often more than $5,000 just for freezing the eggs, in addition to the cost of fertilization.
Vitrification may improve the odds that older women will be able to conceive from eggs that they donated when they were younger, but it doesn’t offer much help to middle-aged women whose eggs were never frozen. There’s little point in a woman preserving her eggs if she’s over 35 years old, when fertility starts to diminish. The younger the eggs, the better their quality.
Still, many fertility centers limit egg-freezing services only to younger cancer patients facing treatments that will leave them sterile. Patients usually are warned that frozen eggs are not as reliable as frozen embryos and sperm because of the egg’s extreme sensitivity to temperature.
“I’ve had to tell young women facing cancer treatment and the loss of ovarian function that it’s not really reliable,” said Dr. Richard Marrs, managing partner of California Fertility Partners in Los Angeles. “The odds are better for them if they freeze embryos.”
Trying to improve the odds, some researchers, including Dr. Silber, have begun freezing not only eggs but ovarian tissue as well. Thin slices from the ovary are removed through a small incision below the navel, preserved with slow freezing, then transplanted back into the woman’s body when she’s ready to try to get pregnant, in some cases years later. The aim is to have the tissue grow and start functioning again, triggering normal ovulation cycles and eventually leading to conception.
The American Society for Reproductive Medicine has acknowledged the potential of frozen eggs and ovarian tissues, but for now recommends these experimental techniques only for younger women undergoing cancer treatments, not for those postponing pregnancy for lifestyle reasons like pursuing a career. “The biological clock is real for most women, and that has to be recognized,” said Sean Tipton, a spokesman for the society.
More widely used fertility techniques that were developed to improve the odds of a successful pregnancy in older women, like pre-implantation genetic diagnosis, or P.G.D., are not without their controversies, too. Developed about a decade ago to weed out embryos with genetic abnormalities prior to implantation, P.G.D. might one day help parents select not just a child’s gender, but perhaps his eye color or other characteristics.
Many reputable clinics find it a slippery ethical slope and employ the procedure only on a limited basis. “We use P.G.D., but we’re very selective when we use it,” Dr. Marrs said. “The prime reason to do it is if you have a family history of single gene disorders like Tay-Sachs, Huntington’s chorea, cystic fibrosis.”
Furthermore, critics claim, P.G.D. may have resulted in clinics discarding healthy embryos. Several studies have shown that many genetic abnormalities appearing in a three-day-old embryo correct themselves by the fifth day. As a result of this finding, a number of clinics now wait until the fifth day to test and transfer embryos into the woman’s uterus. Doctors also tend to transfer fewer of them, thereby reducing the incidence of multiple births and its attendant complications, including premature labor and low birth weight.
Despite these refinements in assisted reproductive technologies, fertility scientists have not been able to change the basic fact that a woman’s fertility diminishes with age.
“The younger the woman, the better her chances of fertility,” said Dr. Zev Rosenwaks, director of The Center for Reproductive Medicine and Infertility at New York-Presbyterian Hospital. “If there are any signs of infertility — absence of periods, irregular periods — couples should pay attention. Seek help earlier rather than later.”
TODAY'S BOOK SUGGESTION:
 It Starts with the Egg:
It Starts with the Egg:How the Science of Egg Quality Can Help You Get Pregnant Naturally, Prevent Miscarriage, and Improve Your Odds in IVF
by Rebecca Fett
-- Whether you are trying to conceive naturally or through IVF, the quality of your eggs will have a powerful impact on how long it takes you to get pregnant and whether you face an increased risk of miscarriage.
Poor egg quality is emerging as the single most important cause of age-related infertility, recurrent miscarriage, and failed IVF cycles. It is also a major contributor to infertility in PCOS.
Based on a comprehensive investigation of a vast array of scientific research, It Starts with the Egg reveals a groundbreaking new approach for improving egg quality and fertility.
With a concrete strategy including minimizing exposure to toxins such as BPA and phthalates, choosing the right vitamins and supplements to safeguard developing eggs, and harnessing nutritional advice shown to boost IVF success rates, this book offers practical solutions to will help you get pregnant faster and deliver a healthy baby.
Click to order/for more info: It Starts with the Egg
Don't have a Kindle? Get your Kindle here, or download a FREE Kindle Reading App.
Photo by bies
 Vaginal Progesterone is Equally Effective in Achieving Pregnancy Outcomes as Injectable Progesterone in Donor Egg Cycles
Vaginal Progesterone is Equally Effective in Achieving Pregnancy Outcomes as Injectable Progesterone in Donor Egg Cycles
A retrospective analysis conducted at a large infertility center evaluated pregnancy outcomes for 225 donor egg recipients
A retrospective analysis of anonymous oocyte (egg) donation cycles, comparing the pregnancy outcomes between vaginally-administered progesterone versus intramuscular (IM) progesterone injections, demonstrates that vaginally-administered progesterone and IM progesterone achieve equal pregnancy outcomes, according to data presented by Brian Berger, MD, Boston IVF, at the Pacific Coast Reproductive Society annual meeting in Rancho Mirage, CA. The retrospective study was supported by a grant from Columbia Laboratories, Inc. (NASDAQ:CBRX).
“We found no significant differences in pregnancy outcomes between patients treated with vaginal progesterone versus progesterone administered intramuscularly,” said Dr. Berger. “Further, vaginal progesterone has the added advantage of avoiding painful intramuscular injections.”
In 225 egg donor cycles, 105 patients received vaginally-administered progesterone (CRINONE® 8% (a bioadhesive progesterone gel)) and 120 received IM progesterone. The implantation rate was 43.8% for vaginal progesterone versus 37.1% for IM progesterone (p=0.175). Recipients treated with vaginal progesterone achieved a 58.1% pregnancy rate and a 51.4% delivery rate, versus a 53.3% pregnancy rate (p=0.503) and a 48.3% delivery rate (p=0.689) for patients receiving IM progesterone. The pregnancy loss rate was 10.5% for patients using vaginal progesterone and 10.8% for IM progesterone users (p=1.00).
“This study clearly demonstrates that vaginal progesterone gel achieves the same pregnancy outcomes as progesterone administered via an intramuscular injection. This is important confirmation that CRINONE® 8% offers patients an efficacious and more convenient option for providing progesterone support in infertility treatment,” Berger added.
Boston IVF is one of America’s most successful fertility centers, providing patients with unparalleled medical care and the best experience with the expertise of premier doctors and professional staff, who are affiliated with Harvard Medical School. It is world renowned for its highly successful and innovative infertility treatments, highest quality service, state-of-the-art methods, ongoing scientific research, and on-site complementary healthcare at its Domar Center.
About Progesterone and Luteal Phase Support
Progesterone is the pregnancy hormone that creates a healthy environment in a woman’s uterus where a fertilized egg can implant and grow into a healthy baby. Most women undergoing infertility treatment need additional progesterone to help prepare the uterus for implantation and development of a fertilized egg.
Before ovulation, progesterone levels in a woman’s body remain relatively low, but rise after ovulation during the latter part of a woman’s menstrual cycle which is called the luteal phase. The luteal phase begins with the production of progesterone and ends with either pregnancy or menstruation, when the uterus sheds its lining. During pregnancy, progesterone helps to maintain the lining of the uterus, providing necessary nutrients to support and nurture a fertilized egg.
Source: http://www.businesswire.com/portal/site/google/?ndmViewId=news_view&newsId=20080414005254&newsLang=en
Life Begins...
Miscarriage stories of loss, hope & help
http://born2luv.blogspot.com/
Stories of Pregnancy & Birth over 44y
- Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
4,550 Stories of Pregnancy & Birth over 44y
Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
Recent Keyword Searches: how to get pregnant over 40, fsh still high but had tubal could i get pregnant, 'i got pregnant at 45, moms over 40, women egg freezing, choosing to get pregnant at 45, can you get pregnant at 45?, women of advanced age pregnant stereotyping, semen quality after age 47, success stories of women having a baby at age 46
 Vaginal Progesterone is Equally Effective in Achieving Pregnancy Outcomes as Injectable Progesterone in Donor Egg Cycles
Vaginal Progesterone is Equally Effective in Achieving Pregnancy Outcomes as Injectable Progesterone in Donor Egg CyclesA retrospective analysis conducted at a large infertility center evaluated pregnancy outcomes for 225 donor egg recipients
A retrospective analysis of anonymous oocyte (egg) donation cycles, comparing the pregnancy outcomes between vaginally-administered progesterone versus intramuscular (IM) progesterone injections, demonstrates that vaginally-administered progesterone and IM progesterone achieve equal pregnancy outcomes, according to data presented by Brian Berger, MD, Boston IVF, at the Pacific Coast Reproductive Society annual meeting in Rancho Mirage, CA. The retrospective study was supported by a grant from Columbia Laboratories, Inc. (NASDAQ:CBRX).
“We found no significant differences in pregnancy outcomes between patients treated with vaginal progesterone versus progesterone administered intramuscularly,” said Dr. Berger. “Further, vaginal progesterone has the added advantage of avoiding painful intramuscular injections.”
In 225 egg donor cycles, 105 patients received vaginally-administered progesterone (CRINONE® 8% (a bioadhesive progesterone gel)) and 120 received IM progesterone. The implantation rate was 43.8% for vaginal progesterone versus 37.1% for IM progesterone (p=0.175). Recipients treated with vaginal progesterone achieved a 58.1% pregnancy rate and a 51.4% delivery rate, versus a 53.3% pregnancy rate (p=0.503) and a 48.3% delivery rate (p=0.689) for patients receiving IM progesterone. The pregnancy loss rate was 10.5% for patients using vaginal progesterone and 10.8% for IM progesterone users (p=1.00).
“This study clearly demonstrates that vaginal progesterone gel achieves the same pregnancy outcomes as progesterone administered via an intramuscular injection. This is important confirmation that CRINONE® 8% offers patients an efficacious and more convenient option for providing progesterone support in infertility treatment,” Berger added.
Boston IVF is one of America’s most successful fertility centers, providing patients with unparalleled medical care and the best experience with the expertise of premier doctors and professional staff, who are affiliated with Harvard Medical School. It is world renowned for its highly successful and innovative infertility treatments, highest quality service, state-of-the-art methods, ongoing scientific research, and on-site complementary healthcare at its Domar Center.
About Progesterone and Luteal Phase Support
Progesterone is the pregnancy hormone that creates a healthy environment in a woman’s uterus where a fertilized egg can implant and grow into a healthy baby. Most women undergoing infertility treatment need additional progesterone to help prepare the uterus for implantation and development of a fertilized egg.
Before ovulation, progesterone levels in a woman’s body remain relatively low, but rise after ovulation during the latter part of a woman’s menstrual cycle which is called the luteal phase. The luteal phase begins with the production of progesterone and ends with either pregnancy or menstruation, when the uterus sheds its lining. During pregnancy, progesterone helps to maintain the lining of the uterus, providing necessary nutrients to support and nurture a fertilized egg.
Source: http://www.businesswire.com/portal/site/google/?ndmViewId=news_view&newsId=20080414005254&newsLang=en
Life Begins...
Miscarriage stories of loss, hope & help
http://born2luv.blogspot.com/
Stories of Pregnancy & Birth over 44y
- Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
4,550 Stories of Pregnancy & Birth over 44y
Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
Recent Keyword Searches: how to get pregnant over 40, fsh still high but had tubal could i get pregnant, 'i got pregnant at 45, moms over 40, women egg freezing, choosing to get pregnant at 45, can you get pregnant at 45?, women of advanced age pregnant stereotyping, semen quality after age 47, success stories of women having a baby at age 46
LONDON - Age is no bar to being a good mother and there is no reason, from the child's point of view, to stop pensioners becoming parents, researchers say.
Women in their 50's and 60's who conceive after fertility treatment are just as capable of being good parents as their sisters in their 30's and 40's.
The research will bring hope to thousands of women who have delayed parenthood and seek help late in life to have a family. Even though they run greater risks of complications during pregnancy and birth, once their children are born they are just as good at raising them.
The finding will also boost research into egg freezing, which could allow career women in their 20s to store their eggs for use in their 40's or 50's or even later. If egg freezing becomes a practical possibility for the average woman, it could fuel a boom in demand for fertility treatment from 40 and 50-year-olds.
Researchers from the University of Southern California studied the mental and physical health of 150 women, a third of whom had become parents in their 50s after in-vitro fertilisation with donor eggs. They found no significant difference in the health or stress levels of the older women that was likely to reduce their parenting capacity compared with younger groups in their 40s and 30s.
All the women gave birth between 1992 and 2004 at a single Los Angeles hospital and were sent questionnaires of which half were returned. On mental functioning, the over-50s were the only group who scored significantly higher than the national average.
The finding goes some way to answering critics of the trend to later motherhood who accuse women seeking fertility treatment in their 50's and 60's of being selfish and ignoring the welfare of their children.
But the study was criticised by a British specialist who said it followed women with children up to the age of 12 and did not show how older mothers would cope in their 60's and 70's when their children reached the more challenging teenage years.
Patricia Rashbrook, from Lewes, who became Britain's oldest mother at the age of 62 last July, defended herself against charges that she would be 80 before her child left school by saying it was the "quality of parenting that matters, not age".
The study from the University of Southern California supports her case.
Anne Steiner, who led the research, said: "The conclusion from this study, though it is limited and of small size, is that if we look from the perspective of stress and physical and mental functioning, it doesn't seem we can restrict parenting based on these reasons."
Rest of the story: http://www.nzherald.co.nz/category/story.cfm?c_id=204&objectid=10407206
Life Begins...
Miscarriage stories of loss, hope & help
http://born2luv.blogspot.com/
Stories of Pregnancy & Birth over 44y
- Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
4,550 Stories of Pregnancy & Birth over 44y
Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
Recent Keyword Searches: is 40 too old to be pregnant, pregnancy age 45 ivf, can you get pregnant when you go through menopause, pregnant in your forties, pregnant at age 46, how likely is it to get pregnant at age 45, can a 42 year old become pregnant naturally, first 48 year old pregnant with own eggs, how old is too old to get pregnant naturally, incidence of birth defects and childbearing in your 40's
Women in their 50's and 60's who conceive after fertility treatment are just as capable of being good parents as their sisters in their 30's and 40's.
The research will bring hope to thousands of women who have delayed parenthood and seek help late in life to have a family. Even though they run greater risks of complications during pregnancy and birth, once their children are born they are just as good at raising them.
The finding will also boost research into egg freezing, which could allow career women in their 20s to store their eggs for use in their 40's or 50's or even later. If egg freezing becomes a practical possibility for the average woman, it could fuel a boom in demand for fertility treatment from 40 and 50-year-olds.
Researchers from the University of Southern California studied the mental and physical health of 150 women, a third of whom had become parents in their 50s after in-vitro fertilisation with donor eggs. They found no significant difference in the health or stress levels of the older women that was likely to reduce their parenting capacity compared with younger groups in their 40s and 30s.
All the women gave birth between 1992 and 2004 at a single Los Angeles hospital and were sent questionnaires of which half were returned. On mental functioning, the over-50s were the only group who scored significantly higher than the national average.
The finding goes some way to answering critics of the trend to later motherhood who accuse women seeking fertility treatment in their 50's and 60's of being selfish and ignoring the welfare of their children.
But the study was criticised by a British specialist who said it followed women with children up to the age of 12 and did not show how older mothers would cope in their 60's and 70's when their children reached the more challenging teenage years.
Patricia Rashbrook, from Lewes, who became Britain's oldest mother at the age of 62 last July, defended herself against charges that she would be 80 before her child left school by saying it was the "quality of parenting that matters, not age".
The study from the University of Southern California supports her case.
Anne Steiner, who led the research, said: "The conclusion from this study, though it is limited and of small size, is that if we look from the perspective of stress and physical and mental functioning, it doesn't seem we can restrict parenting based on these reasons."
Rest of the story: http://www.nzherald.co.nz/category/story.cfm?c_id=204&objectid=10407206
Life Begins...
Miscarriage stories of loss, hope & help
http://born2luv.blogspot.com/
Stories of Pregnancy & Birth over 44y
- Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
4,550 Stories of Pregnancy & Birth over 44y
Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
Recent Keyword Searches: is 40 too old to be pregnant, pregnancy age 45 ivf, can you get pregnant when you go through menopause, pregnant in your forties, pregnant at age 46, how likely is it to get pregnant at age 45, can a 42 year old become pregnant naturally, first 48 year old pregnant with own eggs, how old is too old to get pregnant naturally, incidence of birth defects and childbearing in your 40's
This video tells you all wanted to know about IVF but didn't know whom to ask. So what actually happens in an IVF cycle ? We all know that IVF is expensive - but you still have a hundred questions. Is it painful? Complicated? How do they take out your eggs? How do they put them back? What actually happens in the IVF lab? Here's a guided tour of what going through an IVF cycle involves:
Photo by fcarrero99
fcarrero99
 fcarrero99
fcarrero99ON A SUMMER DAY IN A MINNEAPOLIS SUBURB, Karmin and Steve Eisma watch fondly as their nephew pushes a toy duck down the driveway and their niece peddles a miniature bike with training wheels. The children belong to Karmin's brother, and the childless couple dotes on them. The Eismas are professionals in their early thirties. They long for children of their own. "It just seems like it's so ingrained in me to want a family," Karmin says wistfully.
Karmin describes her yearnings for a baby. LISTEN
Steve nods thoughtfully. "Having a family I think is, or will be, a way to help shape a life," he says. "I'd want the child to be just a very strong person, a good person that has integrity and is a shining light in the world."
The Eismas are infertile because Karmin lost her uterus to cancer in 1991, a few years before they met. They recently tried to adopt a baby, but the birth mother changed her mind a few weeks before the baby was born.
With a remarkable offer from their sister-in-law, Becky, the Eismas are trying high-tech medical treatments that offer a chance to create a child genetically-related to a woman with no uterus. In summer 1997, doctors took eggs from Karmin's ovaries, fertilized them with Steve's sperm, and transferred them into Becky's uterus. Becky offered to be the baby's "gestational carrier," essentially loaning her body -- her womb -- to Karmin. Just before the transfer, the doctor showed Karmin and Steve their laboratory-made embryos under a microscope. "We saw them," Karmin says with awe. "I actually did it after all this. I made ... " She trails off and then says softly, "Those were my babies."
Three of the embryos were transferred to Becky's uterus, but did not survive. The odds were always gathered against them. Only one in three IVF procedures results in pregnancy. Karmin's case was especially difficult because internal scarring from her cancer surgery meant she needed a general anesthetic to have her eggs extracted. When she came to, dizzy and in pain, she said, "I'm never doing this again." She later changed her mind. Having already spent more than $20,000 on legal and clinical services, the Eismas are saving up for another IVF as soon as they can get the money together.
"I remember watching shows where people said they spent a hundred thousand dollars trying to do the IVF and I just said, 'Why would they keep trying?'" Karmin says. "And I know, now. It's very hard to let it go when you actually saw them. And it's a good chance." She pauses a moment and says, "An okay chance."
Donna Shen, president of the Infertility Network in Houston, says infertile people who use assisted reproduction are simply doing what they have to do to have babies. LISTEN
Psychologists say the cycle of hope and despair infertility patients go through can be addictive. It's like playing the slot machines: an occasional small win keeps people dropping quarters in, hoping for a jackpot, even though the odds are with the house and they know it.
Shen says once people start treatment, they may end up spending more than they expected. LISTEN
Dr. Cecelia Valdes, an infertility specialist in Houston, saw a 44-year-old patient recently who asked about the chances of getting pregnant with her own eggs. A female is born with her entire lifetime supply of eggs. Researchers say a woman's fecundity drops precipitously after age 40, largely because of declining egg "quality." Valdes told the patient her chances of success were five percent, at best. The patient answered, "So there's hope."
Valdes will tell her patients the odds, but not when they should give up on treatment. That's the patient's decision, she says. A few decades ago, it was easier for a doctor to tell an infertile couple when to stop. If surgery failed, that was the end of it.
Today, a patient's hopes are rekindled by the steady stream of new developments in reproductive medicine. "What was an experiment last year is a treatment that we're offering a lot of people this year," Valdes says. Just when it seems to a couple that all the medical possibilities have been exhausted, researchers come up with a new solution. That means another expensive chance for people who dream of bearing children.
Source: http://americanradioworks.publicradio.org/features/fertility_race/part2/narr_danger.shtml
Life Begins...
Miscarriage stories of loss, hope & help
http://born2luv.blogspot.com/
Stories of Pregnancy & Birth over 44y
- Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
4,550 Stories of Pregnancy & Birth over 44y
Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
Recent Keyword Searches: pregant at 45, how uncommon is it to be pregnant in your 40s, is 40 too old to get pregnant, get pregnant naturally after age 41, how old can you be and still get pregnant, whole milk bad for fertility over 40, having children in your forties, how to increase sperm production, missed period at 44. can i be pregnant?, wanting to get pregnant older woman
Karmin describes her yearnings for a baby. LISTEN
Steve nods thoughtfully. "Having a family I think is, or will be, a way to help shape a life," he says. "I'd want the child to be just a very strong person, a good person that has integrity and is a shining light in the world."
The Eismas are infertile because Karmin lost her uterus to cancer in 1991, a few years before they met. They recently tried to adopt a baby, but the birth mother changed her mind a few weeks before the baby was born.
With a remarkable offer from their sister-in-law, Becky, the Eismas are trying high-tech medical treatments that offer a chance to create a child genetically-related to a woman with no uterus. In summer 1997, doctors took eggs from Karmin's ovaries, fertilized them with Steve's sperm, and transferred them into Becky's uterus. Becky offered to be the baby's "gestational carrier," essentially loaning her body -- her womb -- to Karmin. Just before the transfer, the doctor showed Karmin and Steve their laboratory-made embryos under a microscope. "We saw them," Karmin says with awe. "I actually did it after all this. I made ... " She trails off and then says softly, "Those were my babies."
Three of the embryos were transferred to Becky's uterus, but did not survive. The odds were always gathered against them. Only one in three IVF procedures results in pregnancy. Karmin's case was especially difficult because internal scarring from her cancer surgery meant she needed a general anesthetic to have her eggs extracted. When she came to, dizzy and in pain, she said, "I'm never doing this again." She later changed her mind. Having already spent more than $20,000 on legal and clinical services, the Eismas are saving up for another IVF as soon as they can get the money together.
"I remember watching shows where people said they spent a hundred thousand dollars trying to do the IVF and I just said, 'Why would they keep trying?'" Karmin says. "And I know, now. It's very hard to let it go when you actually saw them. And it's a good chance." She pauses a moment and says, "An okay chance."
Donna Shen, president of the Infertility Network in Houston, says infertile people who use assisted reproduction are simply doing what they have to do to have babies. LISTEN
Psychologists say the cycle of hope and despair infertility patients go through can be addictive. It's like playing the slot machines: an occasional small win keeps people dropping quarters in, hoping for a jackpot, even though the odds are with the house and they know it.
Shen says once people start treatment, they may end up spending more than they expected. LISTEN
Dr. Cecelia Valdes, an infertility specialist in Houston, saw a 44-year-old patient recently who asked about the chances of getting pregnant with her own eggs. A female is born with her entire lifetime supply of eggs. Researchers say a woman's fecundity drops precipitously after age 40, largely because of declining egg "quality." Valdes told the patient her chances of success were five percent, at best. The patient answered, "So there's hope."
Valdes will tell her patients the odds, but not when they should give up on treatment. That's the patient's decision, she says. A few decades ago, it was easier for a doctor to tell an infertile couple when to stop. If surgery failed, that was the end of it.
Today, a patient's hopes are rekindled by the steady stream of new developments in reproductive medicine. "What was an experiment last year is a treatment that we're offering a lot of people this year," Valdes says. Just when it seems to a couple that all the medical possibilities have been exhausted, researchers come up with a new solution. That means another expensive chance for people who dream of bearing children.
Source: http://americanradioworks.publicradio.org/features/fertility_race/part2/narr_danger.shtml
Life Begins...
Miscarriage stories of loss, hope & help
http://born2luv.blogspot.com/
Stories of Pregnancy & Birth over 44y
- Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
4,550 Stories of Pregnancy & Birth over 44y
Daily blog of hope & inspiration!
http://pregnancyover44y.blogspot.com/
Recent Keyword Searches: pregant at 45, how uncommon is it to be pregnant in your 40s, is 40 too old to get pregnant, get pregnant naturally after age 41, how old can you be and still get pregnant, whole milk bad for fertility over 40, having children in your forties, how to increase sperm production, missed period at 44. can i be pregnant?, wanting to get pregnant older woman
Popular Posts
-
Photo credit: baby aspirin , by looseid Habitual abortions - don't you just love that term??? As if women just have a bad habit of a...
-
Acupuncture appears to be a useful fertility aid, according to a new report in the British Medical Journal that found pairing acupuncture ...
-
Women who began their families later in life share the rewards - and regrets - of delayed motherhood Love, Mom and Me Dr. Abigail Maho...
-
Cigarette smoking appears to have a prolonged, adverse effect on ovarian function. Byproducts of smoking include nicotine and cadmium, which...
-
It's time to update this quote: "In 2009, there were 105,827 live births in the United States to women ages 40 through 44 -- 7...
-
Photo credit: Day 183/365 Doing nothing , by Daniel Oines Many women live through painful periods and discomfort, totally oblivious of t...









Recent Comments